Low grade B cell neoplasms, such as chronic lymphocytic leukemia (CLL), usually are asymptomatic when diagnosed and undergo close observation. Many patients with low grade B cell lymphomas and leukemias (LGBCL) appreciate reassurance that not treating at time of diagnosis is the appropriate management. Society has long focused on diet and lifestyle changes as an alternative to medication; however, there is limited data to which these changes can assist with hematologic disorders.
Green tea (GT) has been studied in regard to its effects on longevity and health. A cohort study followed 52,000 adults over 13 years and found that the frequency of GT consumption was inversely associated with risk of total hematologic neoplasms (Takada M, et al., 2019). There are several other studies that report key oncologic pathways are disrupted by a compound found in GT called epigallocatechin-gallate (EGCG) (Farooqi A, et al., 2020).
Following a case series publication by Dr. Shanafelt, the National Cancer Institute sponsored clinical trials through the Mayo Clinic, evaluating EGCG in 42 patients with asymptomatic CLL. Patients received 2000mg EGCG twice daily for 6 months. Results showed 69% of patients had a biological response with greater than 20% reduction in absolute leukocyte count (ALC) and/or greater than 30% in reduction in size of the lymph node area utilizing standard assessment criteria (Shanafelt T. et al. 2013).
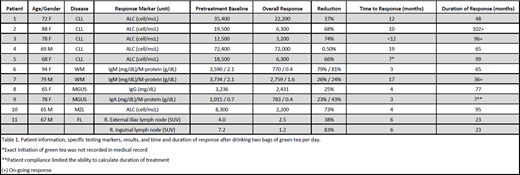
This data encouraged our practice to recommend to patients to drink two bags of GT in steamy hot water daily. We studied 11 patients with indolent CLL, follicular lymphoma (FL), Waldenstrom macroglobulinemia (WM), monoclonal gammopathy of undetermined significance (MGUS), and splenic Marginal zone lymphoma (MZL). No patient was symptomatic. Disease makers were recorded over time during their routine visits for observation. The markers used were ALC for CLL and MZL, standardized uptake value (SUV) on PET scan for lymph node detection for FL, immunoglobulin level as well as monoclonal protein (M-protein) measured by SPEP for MGUS, and IgM and M-protein for WM. One patient with extensive cutaneous plaque psoriasis had routine skin checks. The results were recorded in the electronic health record over varying time periods based on patient presentation and follow up.
Six patients with CLL responded to GT, with reductions in ALC. In patient 1, ALC decreased by 37% over 48 months. Patient 2's ALC decreased by 68% over 102 months. Patient 3's ALC decreased by 74% in 96 months. Patient 4 had a drastic increase in ALC from 23,900 to 72,400 over three years before GT. Once starting GT, his ALC plateaued at 72,000 and has remained stable for 65 months. Patient 5 had decrease ALC of 66% over 99 months.
Patient 6 with WM had a 79% decrease in IgM over 65 months drinking GT. M-protein decreased by 81%. Patient 7 had a decrease in IgM by 26% and a 24% decrease in M-protein over 36 months.
Patient 8 with MGUS had a decrease in IgG by 25% over 77 months. Patient 9 had a decrease in IgG by 23% with M-protein reduction of 43%. Due to compliance issues, duration of therapy was unknown.
Patient 10 with ZL had an ALC reduction of 73% over 95 months.
Lastly, patient 11 with FL and psoriasis was treated with GT for 23 months. There was a reduction of external iliac and inguinal lymph node SUV by 38% and 83% over 23 months, respectively. It was also noted of a significant improvement of extensive plaque psoriasis during this time on GT (Table 1).
The 11 patients highlighted in the practice had improvement in biomarkers and lymphadenopathy during the time they took daily GT. The EGCG study at Mayo Clinic, in which CLL patients took up to 4,000mg of EGCG per day, had significant responses as well as adverse effects including transaminitis. This compares to the population in our study, which includes various types of LGBCL and MGUS that were taking at most 200mg of EGCG per day and had significant responses with no adverse effects. The use of low dose EGCG for inducing clinical improvement of these types of LGBCL and MGUS may be used to delay the onset of starting therapy, thus forestalling immunosuppressive treatment and associated toxicities. Larger randomized control trials involving other forms of indolent LGBCL and MGUS would be significant for the potential of GT being a safe, non-toxic lifestyle change that could benefit patients who do not require aggressive medical therapy for their neoplastic processes.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal